As temperatures rise, heat-related emergencies become a significant concern for emergency medical service (EMS) providers. While most people associate heat-related incidents with dehydration or heatstroke, respiratory emergencies induced by heat exposure are often overlooked. I would like to shed light on the topic of heat-related respiratory emergencies, providing EMS providers with essential knowledge and strategies to effectively manage these cases. Let’s delve into the details and explore the impact of heat on the respiratory system, associated conditions, symptoms, and appropriate prehospital interventions.
The Impact of Heat on the Respiratory System:
Increased respiratory rate: Research has shown that exposure to extreme heat can lead to an increased respiratory rate. This response is the body’s attempt to regulate internal temperature through evaporative cooling, resulting in enhanced water loss through respiration (1).
Dehydration: Heat-related respiratory emergencies are often interconnected with dehydration. Prolonged exposure to high temperatures causes excessive sweating and subsequent fluid loss, leading to dehydration. Dehydration can result in thicker mucus secretions and compromised airway clearance, increasing the risk of respiratory distress (2).
Air pollution: Heatwaves are often associated with an increase in air pollution, including ozone and particulate matter. These pollutants can exacerbate pre-existing respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and allergies, making individuals more susceptible to respiratory emergencies during heatwaves (3).
Heat-Related Respiratory Emergencies and Associated Conditions:
Heat Exhaustion: Heat exhaustion occurs due to prolonged exposure to high temperatures, leading to dehydration and electrolyte imbalances. Symptoms include excessive sweating, weakness, dizziness, headache, nausea, and rapid breathing. Prompt recognition and treatment are essential to prevent progression to heatstroke (4).
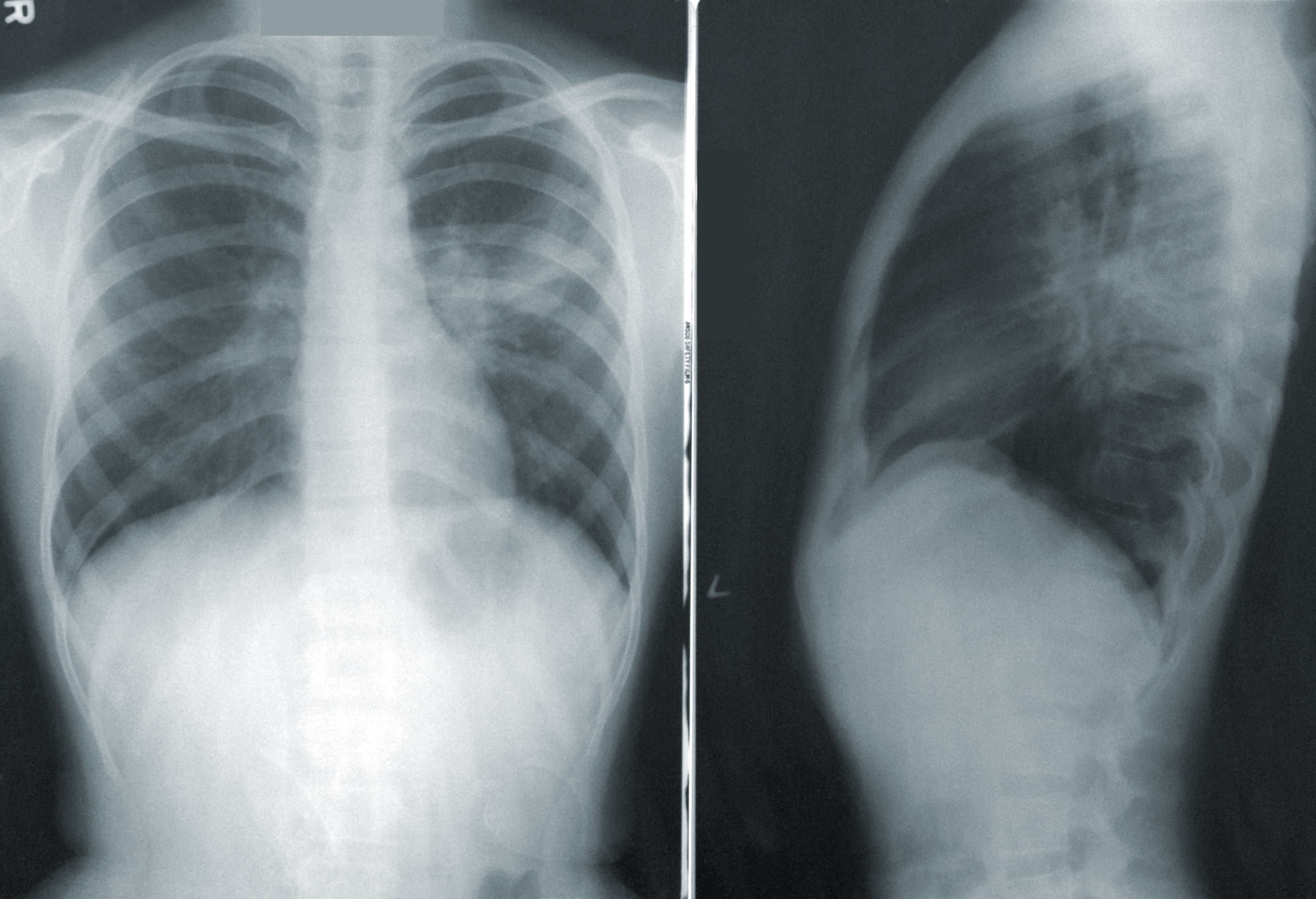
Heatstroke: Heatstroke is a life-threatening condition characterized by a core body temperature above 40°C (104°F) and central nervous system dysfunction. While heatstroke primarily affects the thermoregulatory system, it can also lead to respiratory distress and acute lung injury (5).
Exacerbation of respiratory conditions: Individuals with pre-existing respiratory conditions, such as asthma and COPD, are particularly vulnerable to heat-related respiratory emergencies. Heat and humidity can trigger bronchoconstriction, inflammation, and increased mucus production, leading to respiratory distress (6).
Recognizing Heat-Related Respiratory Emergencies:
Signs and symptoms: EMS providers should be vigilant for the following indicators of heat-related respiratory emergencies:
Rapid, shallow breathing
Shortness of breath
Cyanosis (blue discoloration of lips or extremities)
Altered mental status
Confusion or irritability
Chest pain or tightness
Wheezing or coughing
Patient history: Obtain a thorough patient history, including any pre-existing respiratory conditions, allergies, or medications. This information will guide treatment decisions and help identify potential exacerbating factors.
Prehospital Interventions for Heat-Related Respiratory Emergencies:
Ensure scene safety: Assess the environment for potential hazards and ensure your safety and that of your team before initiating patient care.
Airway management: Administer supplemental oxygen to improve oxygenation. Be prepared to manage airway compromise and consider advanced airway techniques if necessary.
Fluid resuscitation: Assess the patient’s hydration status and initiate fluid resuscitation as needed, following local protocols. This will help correct dehydration and restore electrolyte imbalances.
Active cooling: Employ external cooling measures, such as removing the patient from the heat source, applying cool water or ice packs to the body, and using fans or air conditioning, to lower the patient’s core body temperature.
Symptom management: Treat associated symptoms such as bronchospasm with appropriate medications, including bronchodilators and corticosteroids, based on the patient’s history and local protocols.
Conclusion:
Heat-related respiratory emergencies pose a significant risk during periods of extreme heat. EMS providers play a crucial role in recognizing, assessing, and managing these cases effectively. By understanding the impact of heat on the respiratory system, recognizing associated conditions and symptoms, and employing appropriate prehospital interventions, EMS providers can provide timely and effective care to those experiencing heat-related respiratory emergencies. Stay informed, stay vigilant, and remember to prioritize patient safety and well-being during these challenging situations.
References:
Semenza JC, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84-90.
National Safety Council. Heat exhaustion and heatstroke: 10 tips to keep you safe. Available from: https://www.nsc.org/home-safety/safety-topics/heat-exhaustion
Gent JF, et al. Association of pediatric asthma severity with exposure to common household dust allergens. Environ Res. 2009;109(7):768-774.
Centers for Disease Control and Prevention. Extreme Heat: Heat Exhaustion. Available from: https://www.cdc.gov/disasters/extremeheat/warning.html
Leon LR, et al. A Brief History of Heat Stroke Physiology and the Doctrine of Bioradioation. Compr Physiol. 2015;5(2):611-647.
Zhao Q, et al. Heatwaves and the Exacerbation of Air Pollution: A Narrative Review and Implications for Public Health. Int J Environ Res Public Health. 2015;12(6):7241-7251.