Subdural hematomas (SDHs)—particularly chronic and subacute—are a common neurosurgical challenge, especially in the elderly population. As EMS providers, we frequently encounter patients with signs and symptoms that may point toward SDH: headache, confusion, focal neurological deficits, or a history of recent falls. While our role focuses on identification and rapid transport, understanding the evolving landscape of treatment can enhance our clinical perspective and our communication with receiving facilities.
A recent clinical study published in The Journal of Neurosurgery explored a novel method for managing subacute and chronic SDHs: the use of an intraosseous (IO) needle for bedside decompression. Conducted at Royal Columbian Hospital in British Columbia, this single-center, retrospective review evaluated 51 patients treated with IO decompression over an 18-month period.
Here’s what EMS professionals might find noteworthy:
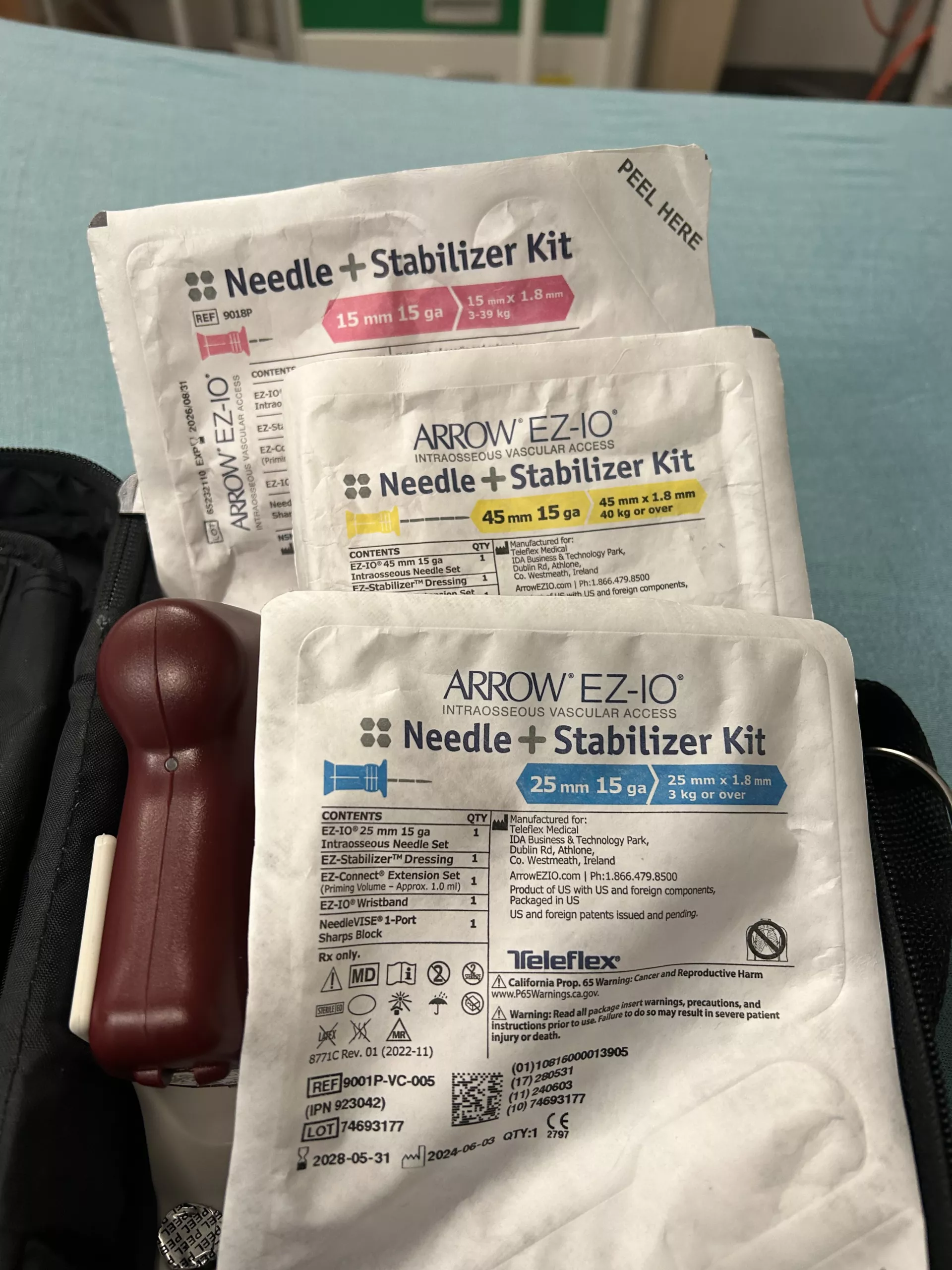
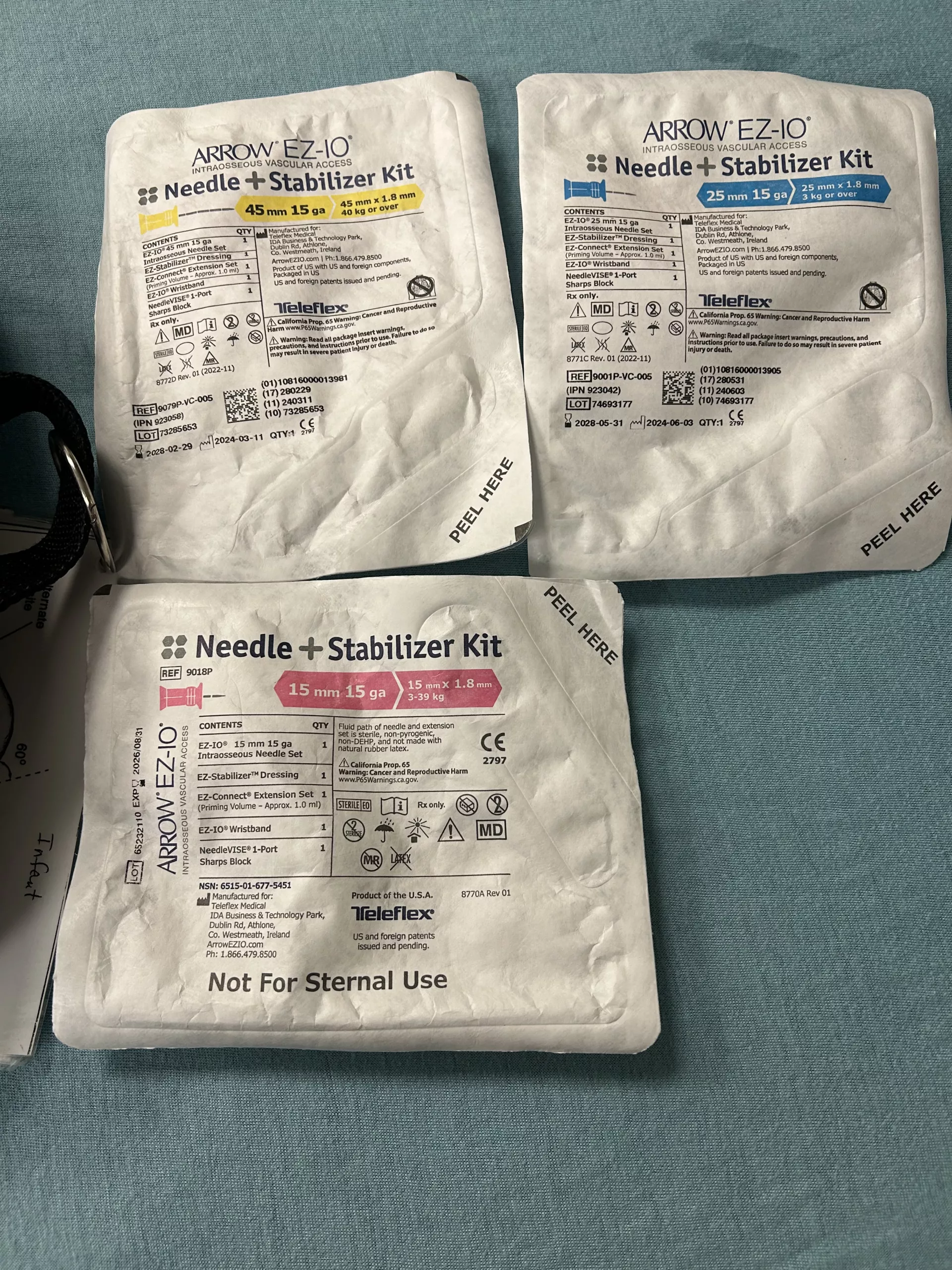
🔹 Technique Overview: Using a standard 15-gauge IO needle, the neurosurgical team performed bedside drainage of the hematoma under local anesthesia. A suction bulb was attached to provide continuous negative pressure, and imaging confirmed hematoma reduction. No general anesthesia or operating room was required.
 Heran, N., MD, Yan, T. D., MD, & Heran, M. K., MD. (2025, May 2). Intraosseous needle for management of subacute and chronic subdural hematoma. Journal of Neurosurgery. Retrieved May 13, 2025, from https://doi.org/10.3171/2025.1.JNS241265
Heran, N., MD, Yan, T. D., MD, & Heran, M. K., MD. (2025, May 2). Intraosseous needle for management of subacute and chronic subdural hematoma. Journal of Neurosurgery. Retrieved May 13, 2025, from https://doi.org/10.3171/2025.1.JNS241265
🔹 Patient Population: The average patient age was 75 years, and most presented with symptoms such as confusion, weakness, headache, or a fall. About one-third had subacute SDHs, and two-thirds had chronic collections.
🔹 Outcomes: Technical success was achieved in all 51 patients. Only one recurrence was reported. Complication rates were low, with minor adverse events like a seizure, blurry vision, or a remote new intracranial hemorrhage occurring in a few cases. There was one reported death, but it was unrelated to the procedure.
🔹 Why This Matters: The conventional treatment for SDH, burr hole craniotomy (BHC), is effective but not without risk. It requires a sizable opening in the skull, carries higher rates of recurrence, and is associated with surgical complications. This IO-based approach offers a minimally invasive alternative with a smaller entry site and fewer complications—at least for the selected patient population in this study.
🔹 EMS Takeaway: While this is not a prehospital technique and isn’t being considered for EMS application, it’s valuable for providers to stay informed about new developments in hospital-based care. Understanding how SDHs may be managed upon arrival can improve handoffs, help frame discussions with families, and reinforce the importance of rapid recognition and transport for altered mental status, especially in older adults.
This study adds to the growing body of research exploring safer, more efficient ways to manage common neurosurgical emergencies. For EMS, it reinforces the value of early recognition and highlights the ongoing evolution of care beyond the ambulance doors.
Take a look at the study: