Thermal burns occur with alarming frequency. Nearly a half a million americans suffer burn injuries severe enough to require specialized burn care annually. Of those, approximately 3500 adults and children suffer fatal burns, this works out to just under 10 fatalities per day. Add that to the number of individuals who suffer smoke inhalation or other gas inhalation and it’s easy to see the importance of understanding the importance of being proficient in identifying the various depths of thermal burns that an burn patient may suffer. The skin is the largest organ in the human body and most thermal burns can be broken down into zones of burn based on the severity and depth of the skin layer involved (cutaneous, subcutaneous, dermal and sub dermal layers). The body responds differently to each zone or depth of tissue that is involved in the burn. Typically the innermost burn region receives the greatest depth of burn and damage, this zone is referred to as the zone of coagulation and often will have the largest area of irreversible tissue damage. The middle layer is identified as the zone of stasis and while it initially may look non salvageable, it can often be largely salvaged by utilizing proper burn care interventions. The outer layer is called the zone of erythema or hyperemia and frequently is the area of tissue that is most readily able to recover from the thermal burn process. Think of these zones as a bullseye on a target.
Skin burn classification infographic medical educational scheme poster isometric vector illustration. Physical injury chemical burning epidermis structure first second third and fourth degree
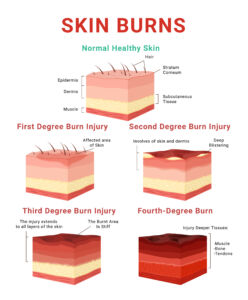
Burns can also be classified by the depth of the burn itself. The shallowest burn depth is referred to as a superficial (formerly first degree) burn. Think of a bad sunburn as an example of a superficial burn Superficial burns involve the outer most skin layers and are normally painful but rarely leave permanent scarring. These burns usually heal completely within 3-6 days. What used to be referred to as second degree burns are now referred to as either Superficial Partial Thickness or Superficial Deep Thicknesss burns. Superficial Partial Thickness burns are often a result of scald or short duration flash thermal burns and are accompanied by red, moist, weeping or blistered skin and are extremely painful as nerve endings are partially involved. Superficial Partial Thickness burns often heal with minimal to no scarring in 1-3 weeks. Deep Partial Thickness burns are deeper into the tissue and may present with the same signs and symptoms as Superficial Partial Thickness burns but may also present with patchy, cheesy white looking areas of skin that rarely will blanch when pressure is applied. These burns typically heal slower and often will cause minor to moderate scarring. Full Thickness burns involve subcutaneous, dermal and sub dermal layers of the skin. This depth of burn destroys much of the epidermal, dermal and sub dermal structures such as sweat glands, sebaceous (oil) glands and nerve endings. Full Thickness burns result in generally less perceived pain due to the fact that nerve endings are irreparably damaged and may require skin grafts, prolonged rehabilitation and may cause significant scarring even with aggressive burn treatment.
Thermal burns have both short term and long term consequences. It is sometimes difficult to accurately identify which depth of burn has been inflicted in the immediate period just after the burn occurs. By having a general knowledge of not only burn depth but the basic burn zones, the EMS provider can aggressively treat and hopefully limit the extent of non salvageable tissue. Regardless of the depth of the burn, if it is not accurately identified and appropriately treated, the short term and long term negative effects of a thermal burn will be magnified.

