This is not an ago old question in medicine as the standard of care in any emergency department or trauma bay is to cut the chest and place a chest tube. However given the means by which EMS operates only recently have we been posed with a question, should we be doing finger thoracostomies (FT) or continue to use the needle decompression (NT) as a treatment for tension pneumothorax?
To look at this question first let’s identification of tension pneumothoraxes’ (PTX) pathology, and when we know we need to act. Absolute indications for treating a PTX:
- Traumatic cardiac arrest where chest trauma is present
- Hypoxia <92 refractory to supplemental O2 in the presence of chest trauma
- Hypotension MAP <65 / SBP<90 where chest trauma is present
- Difficulty ventilating (i.e. elevated peak inspiratory pressures, increased resistance to bag-valve ventilation) where tension PTX is the suspected etiology
- Jugular vein distention
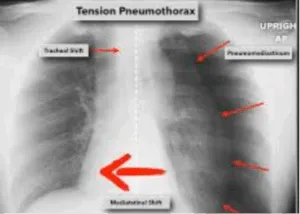
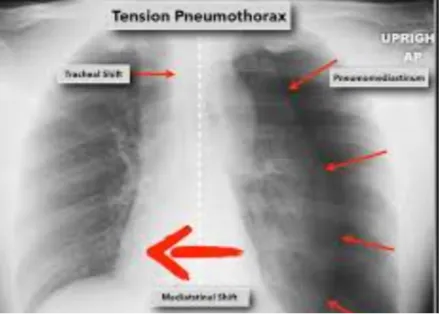
- Deviated trachea
Some things to remember with these indication, hypoxia, hypotension and tachycardia should come together, hypotension without hypoxia may be more concerning for hypovolemic shock. Difficulty in ventilation for the intubated patient should follow the DOPE pneumonic rule out obstruction Via suctioning first. (Dislodged ETT should alarm for low inspiratory pressures.) As always, a deviated trachea is a laten sign of a PTX. But it is also rarely present with some studies suggesting it is present in less than 50% of cases identified by paramedics. Other studies find it present in less than 25% of cases overall. Where as 90% of cases have acute chest pain and 80% have dyspnea. While definitive diagnosis in the ED Via a chest X-ray is the likely course of action for in hospital cases, EMS doesn’t have that luxury and we should not wait to arrive at the ED with a patient who shows tension pathology. One up and coming tool that can help reassure an EMS provider would be ultra sound (POCUS). With POCUS we can exam the ribs and lungs looking for lung slide, if no lung slide is present at a minimum we can have a pneumothorax, tension pneumothorax or potential a hemothorax.
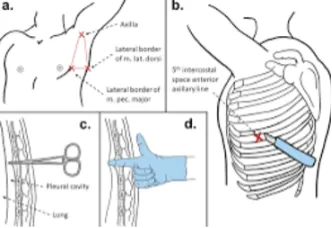
Now that we have identified when a tension pneumothorax is present and the need for action lets describe the steps needed to complete a FT.
Open “simple” Thoracostomy (Finger Thoracostomy)
- Utilize universal precautions including face, eye protection and sterile gloves if available ii.
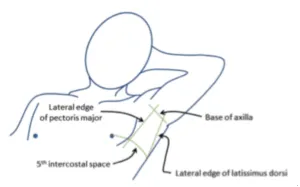
- With arm abducted, find and mark the area at the anterior 4th or 5th intercostal space at the anterior or between anterior & mid-axillary line within the triangle of safety
- Clean the area with a chlorhexidine prep stick
- Make a 2-3 inch transverse incision through the skin along the 4th or 5th rib, anterior axillary line in the triangle of safety utilizing scalpel (#10 preferred).
- Utilizing curved hemostats, ride the superior aspect of the rib and then penetrate parietal pleura
- Penetration is accomplished with a gently, steady push (while feeling for a sudden “give” or “pop”)
- Depth should generally NOT exceed 3 cm past targeted rib
- USE CAUTION. Contents in thoracic cavity MAY BE UNDER PRESSURE
- Forcefully open the hemostats to bluntly dissect intercostal muscle wide enough to carefully insert finger into pleural cavity. Avoid closing the hemostats once opened.
- Withdraw the open hemostats to further dissect the incision
- Insert finger along the track into the pleural cavity and perform sweep
- Ensure that adhesions between parietal and visceral pleura (if present) are gently released (Be careful as there may be fractured ribs with jagged edges that may puncture glove/skin)
- Remove finger and monitor patient for improvement or complications.
- Each wound should be circled with a permanent marker and labeled EMS to identify incisions made by EMS
- Consider vent chest seal if patient spontaneously breathing
- Administer Cefazolin (Ancef) 2g IV/IO over 5 min (or another broad-spectrum antibiotic as per state/local protocol)

Some things to remember about the FT, in general this is for adult patient >14 years of age, land marks must be easily identifiable and perhaps most importantly a vented chest seal should be available and strongly considered. Quality metrics from a QA perspective should include the rapid recognition of tension/shock pathology along with the time from recognition to the time of completed management. Whether using a needle or a finger if properly completed an easing in respiratory distress should be noted and hypoxia should be corrected. Hypotension and tachycardia however may remain if the patient is also in hypovolemic shock, and stagnant hypoxia may persist as well. Ensure that you continue to follow your trauma protocol with the administration of blood product and TXA to address these concerns.
In order to answer the initial question, should EMS be using FT over NT, we should compare and contrast the effectiveness of the NT with FT. While the research is still new and therefore limited one such study found that of 34 participants, with 15 receiving FT and 19 receiving NT, the finger group had a 93.3% success rate of intrathoracic decompression, compared to the needle group which saw a 47.7% success rate. However, when accounting for the severity of injuries and survival rate post initial resuscitation the in-hospital mortality rate shows no significant difference (P=0.213). There are several limitations to this study however, the most prominent being the small sample size of 34. Further more the paper highlights that no autopsies were performed on any of the participants limiting the ability to determine fatal complications related to the procedure. Although imaging did find one participant in the needle group to have a subclavian artery injury, where as no injuries to the great vessels or thoracic organ were found in the finger group. Given these limitations it would be unwise to speak to the safety of FT v.s. NT. The largest study to date (as of 2015) looking at FT in the prehospital setting was conducted in Europe by a Helicopter EMS physician-based service. 126 patients were included with 236 finger thoracostomies performed (bilateral PTX) showed a significant improvement in SPO2 readings from an average of 91% to an average of 97% at the time of patient arrival in the trauma bay. There were no documented immediate complications from the procedure. However, the study did not compare and contrast the effectiveness of needle decompression and the provider performing the intervention was an EM trained physician not a paramedic. This also leads to the need for further research on the safety of FT in the pre-hospital field.
In conclusion given the limited amount of research that directly looks at NT v.s. FT we can only conclude that FT tends to be more successful as a procedure. While many studies differ on the percentage all that were examined had a significantly higher success rate of decompressing the tension pneumothorax. However limited data exist to suggest the safety of the NT v.s. FT. Obviously the risk to providers given the use of a scalpel the presence of potentially broken ribs or bone fragments is higher. Keeping these studies in mind coupled with my own personal experiences I would argue that finger thoracostomies will continue to grow in pre-hospital popularity but I doubt we will see it become the standard of care for some time, if at all, across the country; given the invasive nature and the relative rarity that individual paramedics perform the skill. As always refer to your state and local protocol as this blog is merely educational in nature and also opinion based.
References
Chesters, A., Davies, G., & Wilson, A. (2015). Four years of pre-hospital simple thoracostomy performed by a physician-paramedic helicopter emergency medical service team: A description and review of Practice. Trauma, 18(2), 124–128. https://doi.org/10.1177/1460408615619197
Ciaraglia, A., & Smith, A. (2024). COMPARISON OF OUT OF HOSPITAL FINGER AND NEEDLE THORACOSTOMY PERFORMED BY GROUND EMERGENCY MEDICAL SERVICES . International Journal of Paramedicine . https://internationaljournalofparamedicine.com/index.php/ijop/article/view/2820/2778