If you want to be a good paramedic you need to be able to effectively and accurately read a 12-lead. If you want to be a great paramedic you have to be able to interpret 12-leads. What does that mean, it means more than just identifying the standard ST elevated myocardial infraction (STEMI). With that in mind it’s important to identify some topics that aren’t always covered or explained in initial paramedic education.
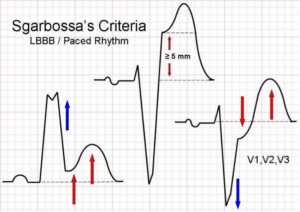
Sgarbossa criteria may be something that you have heard of or may even be something that was briefly discussed in medic school. But it’s going to be important especially in the critical care world, as it’s a set criteria for identifying STEMI’s in the presence of a left bundle branch block (LBBB). Dr. Elana Sgarbossa using data from the GUSTO-1 trial (1993) successfully identified a set of 3 criteria, by which a greater than 90% specificity, can show the presence of a STEMI in the setting of a LBBB. The criteria which were found are as follows:
1. Concordant ST elevation- Meaning that the QRS and the ST segment go in the same direction. >1mm ST elevation in any lead with an upright QRS. (5 points)
2. Concordant ST Depression in leads V1, V2, V3, >1mm ST depression (3 points)
3. Discordant ST elevation- Meaning the QRS is depressed while the ST segment is positive. > 5mm of ST-elevation (2 points)
In order to be shown as a positive result a total of at least 3 points are needed.
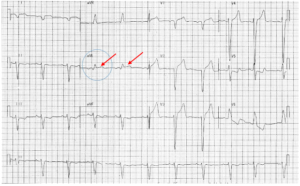
Along with sgarbossa criteria it is important to be able to identify the more subtle posterior STEMI. This is characterized by ST depression in leads V1, V2, V3, along with tall R-waves and upright T-waves.
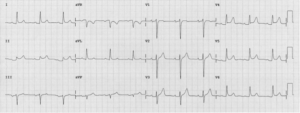
Standard 12-lead note both the ST-depression in leads V1, V2, V3 along with ST elevation in the inferior leads as well.
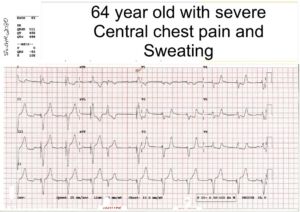
A posterior view confirming an inferior-lateral- posterior STEMI
Soley posterior STEMI’s are rare making up only 3%-11% of STEMI’s. While posterior STEMI’s seen in conjunction with a primarily inferior and/or lateral STEMI’s occur 15-20% of the time. Once we see the indications of a posterior STEMI the way to positively identify the posterior involvement is to simply move leads V4, V5, and V6 to the back and reshoot the 12-lead marking the lateral leads as V7, V8, and V9 and looking for ST elevation.
Is identifying either a posterior STEMI or Sgarbossa criteria going to change our course of treatment, the short answer is no. We should still be transporting the patient to a STEMI capable facility or utilizing air medical to move the patient to definitive care and following our local protocol. When available the transmission of the 12-lead is still important so that the emergency department can appropriately activate the cath lab and prepare for the patient. It’s highly recommended to follow up with the ED via phone and explain your findings especially when it is not immediately obvious. In general, expect the patient to receive the following interventions prior to catheterization.
324mg of ASA
0.4mg Nitroglycerin or a nitro infusion
60U/Kg of heparin (followed by an infusion)
Plavix or brilinta
* There has been usage of TNK or TPA
*Many of these are critical care interventions and can be performed by flight crews
While sgarbossa criteria and the ability to identify a posterior STEMI are important paramedic skills, the ability to recognize when questionable 12-leads including those that may have ST-elevation are not STEMI’s is equally important. There are 9 common STEMI imitators which should be understood to avoid false positive STEMI alerts. The easiest pneumonic to memorize this is ELEVATION.
1. E electrolytes (hyperkalemia)
2. L Left Bundle Branch Block
3. E early repolarization
4. V Left Ventricular hypertrophy
5. A aneurism
6. T Thailand (brugada) syndrome
7. I inflammation (pericarditis)
8. O Osbourn waves (hypothermia)
9. N non-ischemic vasospasm
Let’s discuss Left ventricular hypertrophy and Pericarditis. Left ventricular hypertrophy has several causes to include, hypertension, hypertrophic cardiomyopathy or aortic valve stenosis to name a few. There are several ways to identify this on an EKG to include the Cornell criteria, the modified Cornell criteria, as well as the Sokolow-Lyon criteria and the Romhilt-Estes LVH point score system. By far the easiest to memorize for the pre-hospital provider is the modified Cornell criteria which essential allows you to identify LVH if the R-wave is greater than 12mm in length.
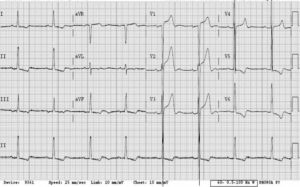
Note there is ST elevation in V1, V2, and V3 but with LVH present this is not a STEMI.
Pericarditis is the swelling and irritation of the pericardium. It commonly causes chest pain which can even radiate to the arms or jaw. However other common symptoms include coughing, and a low-grade fever which are not seen in STEMI’s. It is commonly caused by infections, inflammatory disorders, or acute injury to the chest or heart (previous MI). The characteristic EKG finding is wide spread ST-elevation with reciprocal ST-depression in AvR. A strong assessment can help determine a past medical history which can raise your suspicion for pericarditis Vs STEMI.
As the old joke goes if you were to ask six cardiologists to read an EKG you may very well come out with six different interpretations. Remember the basics of how to read an EKG and how to find a STEMI but always remain open to learning and continue to research and learn throughout your career as a paramedic. That’s the real trick to being a competent and trust worthy provider.
References
Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators – PubMed (nih.gov)
IS IT A STEMI? ST-ELEVATION MYOCARDIAL INFARCTION AND ITS EQUIVALENTS — Louisville Lectures
Posterior Myocardial Infarction • LITFL • ECG Library Diagnosis
STEMI mimics – WikEM