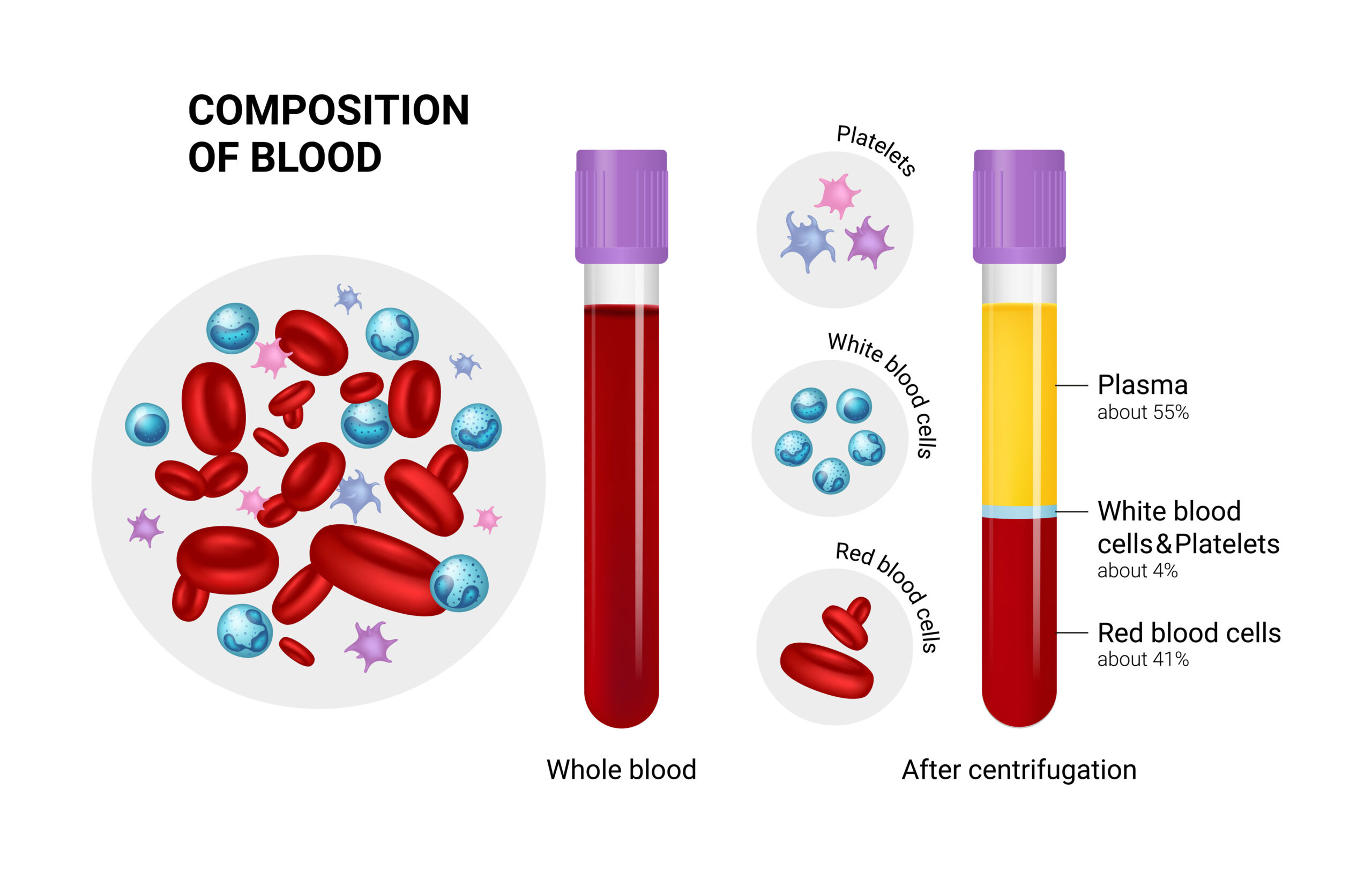
When we think about our blood, most health care providers agree that it is necessary to perfuse our body and losing too much will not be good for our patient. But what is blood and why do we need it? This question has many correct answers. Human blood is not only responsible for providing nourishment and oxygenation to the cells of the body’s organs but it also plays a role in fighting off infection, promoting clotting and regulating body temperature. Human blood is made of four basic components: red blood cells, white blood cells, platelets and plasma. Each of these components play a vital role in maintaining homeostasis within our body. Overall blood volume in relation to body mass is also an important part of discussing the importance of human blood on overall functioning of the body.
Lets start with red blood cells or erythrocytes. Red blood cells are mostly produced in the bone marrow of our bones and have a life span of approximately 120 days or four months. The hemoglobin (Hgb) portion of red blood cells is the primary way oxygen (O2) is carried throughout the body to nourish the cells and carbon dioxide (CO2) is carried away from the cells for removal. Hemoglobin is mostly made up of the element iron (Fe) and is NOT specific for just carrying oxygen. The Hemoglobin molecule has an affinity 250 times greater for Carbon monoxide (CO) than it does for O2. Carbon monoxide is commonly a byproduct of the combustion of fuels such as gasoline, wood, charcoal, kerosene, oil and natural gas. Because the Hgb portion of red blood cells prefers CO over O2, the CO molecule will more readily and rapidly load onto the Hgb molecule until it is completely saturated with CO. Standard oxygen saturation (SPO2) monitors only measure the overall saturation of this molecule and are not specific for just oxygen loading so in the presence of suspected CO poisoning, we should always assume the Hgb molecule is actually loaded either partially or completely with CO and not O2. A normal red blood cell count is 4-5 million and tends to be slightly higher in men than women. Anemia is the term used to describe a lower than normal red blood cell count. Eating foods such as red meat, poultry, shellfish, peas beans and green leafy vegetables have been known to increase a persons red blood cell count.
White Blood Cells (WBC) or Leukocytes are the workhorse of the body’s immunological system and work in concert with other functions to fight off pathogens and disease. The life span of a WBC is between 12 and 20 days and like the red blood cells are manufactured in the bone marrow. They are stored in the spleen and lymph nodes and released when the body responds to an infectious invader. Immature WBC’s are called neutrophils and are constantly being made in the bone marrow of human bones, these neutrophils are the earliest form of WBC to respond to fight off invasion of the body by viruses, bacteria or other foreign invaders. Normal WBC range is 5-10, 000 WBC per microliter and early on in an infectious process the WBC elevates as the body responds to the invader by making additional WBC to assist in fighting off this invasion. Over time, if the infectious process is either not recognized or not treated, the WBC count will decrease due to the fact that these WBC’s are used up faster than the body can make them. Conditions like Leukemia, HIV/AIDS, Hepatitis A and B, Lupus, Rheumatoid Arthritis, Radiation and Chemotherapy all have been proven to lower the overall WBC count. This makes the patient more likely to unable to mount an effective immune response when exposed to an infectious pathogen.
Platelets or thrombocytes are primarily responsible for preventing or stopping bleeding when the body’s blood vessels are damaged. They respond to the site of the disruption and clump together to form a temporary clot in an attempt to slow or stop the bleeding. A normal platelet count is between 150 and 400 thousand platelets per microliter. The lifespan of a platelet is only 7-10 days and this short lifespan is why physicians often advise patients taking anti platelet medications to stop taking them 7-10 days prior to elective surgeries or procedures. A decrease platelet level can lead to increased risk of bleeding even with a minor injury and easy bruising. Like RBC’s and WBC’s, platelets are made in the body’s bone marrow cavity. Interestingly, during fetal development, platelets are not manufactured in the bone marrow but actually are mainly produced in the fetal liver. Platelets are depleted when the body is exposed to a bacterial or viral infection or when the patient uses alcohol or is exposed to chemicals such as arsenic, benzene or certain pesticides. Eating any iron rich food has been proven to increase platelet levels over time.
Plasma is the “liquid portion” of the blood components. It is the medium that carries the platelets, red blood cells and white blood cells throughout the human body. Plasma makes up around 55% of total blood volume. It is made up of salts, enzymes and water. It is often described as having a yellow or stray colored appearance. Decreased plasma levels have been attributed to conditions such as cirrhosis, Hepatitis, chemotherapy treatment, HIV/AIDS, Lupus or alcohol use. Foods such as green leafy vegetables, fatty fish, citrus fruits and iron rich foods have been proven to increase circulating plasma levels.
The overall volume of blood circulating within the body is as important as the individual components listed above. Normal adult circulating blood volume within the vascular system is approximately 5 liters. Blood volume is regulated by the kidneys to maintain the ideal blood volume level within a narrow range. Pediatric patients have a much lower circulating blood volume level and therefore are more likely to be affected by rapid blood loss. A full term 6-8 pound newborn only has only 300-400 ml of blood within the vascular system. This is the equivalent of 12 ounce can of soda. Blood volume can be lost chronically in conditions such as GI bleeds, stomach ulcers, endometriosis or cancer conditions. The body tends to compensate better in situations in which the blood loss is gradual. Rapid or acute blood loss can be caused by traumatic events, aortic ruptures, ruptured ectopic pregnancies and disseminated intravascular coagulation.
As we talked about in part one of this series, adequate perfusion relies on an intact pump (the heart), intact pipes (the blood vessels) and adequate amount of circulating fluid (the blood). While the human body is very aggressive in attempting to compensate for acute blood loss by vascular constriction, increasing cardiac output and shunting blood to the core of the body where the majority of vital organs are located, it can only compensate for a finite amount of time. Once the compensatory mechanisms have been exhausted or overcome, decompensation will occur. The earlier we can identify and begin to treat blood volume loss, the better the chances of survival and/or complete recovery from the insult. Early recognition and a high index of suspicion goes a long way toward preventing decompensation and decreasing mortality and morbidity related to acute blood loss.