The pediatric trauma patient is one of the most challenging calls you may run on in our careers.
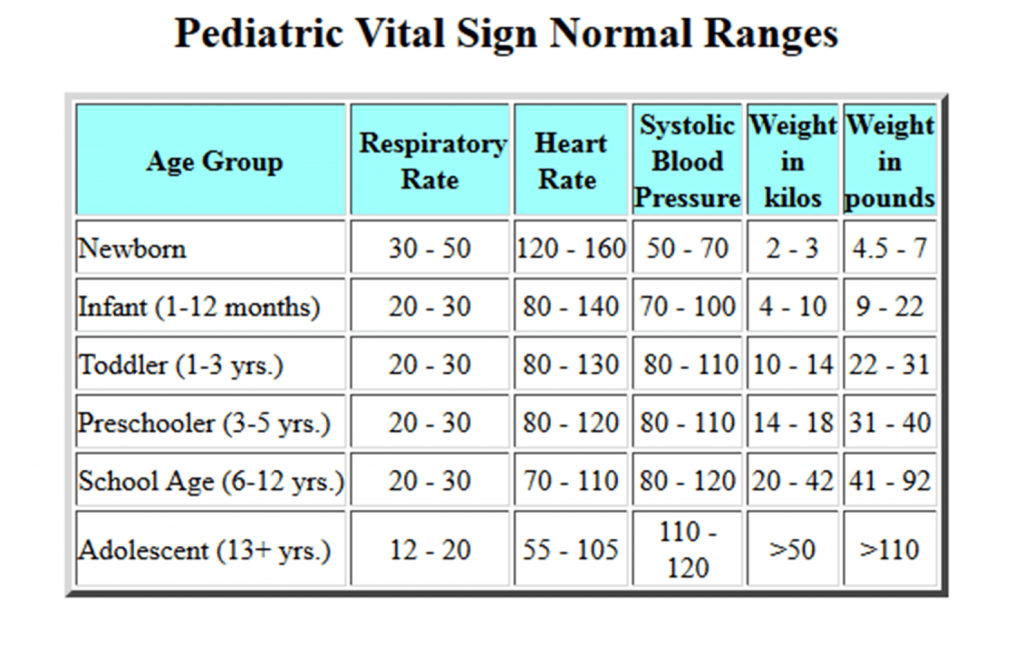
When you are faced with these situations, it is important for you to be able to recognize the signs and symptoms of impending shock in pediatric trauma patients and intervene rapidly. Children will attempt to compensate and do it well, but only for a short period. While they are compensating they may seem unaffected. Thus, it’s important for you to know the normal vital sign ranges for all age groups of the pediatric population.
In order to recognize and treat shock in the pediatric patient, you must first understand what’s occurring within the body. During the initial stages of shock, the patient may exhibit an increase in respiratory rate and heart rate. Blood pressure remains unaffected at this time. Once cardiac output becomes impaired, vasoconstriction occurs as a compensatory measure. Systemic vascular resistance increases and, if left untreated, will cause tissue ischemia.
Early on, microvascular changes occur in which the pre- and post-capillary sphincters constrict. This leads to tissue ischemia and the anaerobic phase of metabolism. A buildup of acid is produced during this anaerobic phase. The pre-capillary sphincters relax and the post-capillary sphincters remain open, creating impaired blood flow through the capillary beds.
Lastly, the post-capillary sphincters relax and allow the metabolites to wash out, then microemboli are released which creates an infarction of the organs, worsening acidosis and eventual patient death.
Facts to keep in while treating pediatric trauma
Traumatic injuries are unfortunately common
Traumatic injuries in pediatrics are the leading cause of death in children ages 1 to 14, according to Childhood Injury: State-by-state mortality facts by Baker and Waller, 1989, The Johns Hopkins Injury Prevention Center.
The risk of traumatic injuries in children increases in certain situations such as families experiencing times of crises or in certain socioeconomic situations.
The most common areas that you may encounter pediatric injuries are:
- Streets — Pedestrian versus car for younger children, while motor-vehicle collisions are more common for older children. Infants have a higher mortality rate resulting from motor-vehicle collisions when they are not properly restrained. Bicycle accidents also are common traumatic injury culprits for younger children.
- Home — Pediatric patients from 2 to 3 years of age suffer more injuries from falls in the home. They also tend to pull things down from shelves or tables. Hot liquids on the stove are of particular concern, as well as toy safety.
- Schools — Physical education activities are one of the leading causes of school-ground injuries in younger children. As children enter the adolescent years, sports-related injuries become more common.
Children’s anatomy differs adults’
The differences in children’s anatomy and physiologic response verses that of an adult plays a significant role in their reaction to trauma. Children tend to suffer more blunt injuries than penetrating. However, their injuries are often more severe because of the concentrated nature of the blunt energy transference.
They have larger heads in relation to their body, which makes them more prone to forward falls. They tend to suffer more diffuse axonal injuries as opposed to subdural, intracranial bleeds and epidural bleeds.
Their spines have more elasticity, but they have weak ligaments holding the spine in place. This makes them more prone to SCIWORA (Spinal Cord Injury Without Radiological Abnormality) injuries, as opposed to actual fractures of the spine.
Airways in children are smaller in diameter. Intubation can be challenging because their epiglottis is floppy and U-shaped. They have smaller functional residual capacity, and the primary means for increasing their minute ventilation is by increasing their respiratory rate.
Early recognition and treatment of respiratory distress is critical in the pediatric patient since it is the primary source of cardiac arrest in children.
Blood pressure in children is not a reliable tool in estimating blood loss
A pediatric patient may lose up to 50% of their blood volume before there is a significant change in their blood pressure.
The earliest sign of blood pressure change is when the diastolic drops slightly. This is a strong indicator of impending shock. The heart rate will typically increase before the systolic drops.
That said, it is important for us to know the acceptable blood pressure ranges and basic formulas for pediatrics. An example is 70 + 2 (age). Keep in mind this is the number you begin treating the patient for hypotension. Example: 4-year-old patient – systolic of 78 is where we begin treatment, not waiting until the systolic drops to 77.
The best measurements of perfusion are to check for peripheral pulse rate, quality and strength:
- A weak, barely palpable radial on older children, or the same for the brachial in infants is an indicator of circulatory impairment.
- Capillary refill time of greater than 2 seconds indicates poor perfusion.
- Abnormal skin color and temp, such as mottled skin, pallor or pale skin, also are indicators of poor perfusion.
- Urine output is one of the most crucial things you can monitor in children since it is an even stronger early indicator of impending shock than blood pressure. Urine output should be 1 to 2/ml/kg in children, but it will drop when the blood volume is less than 25%.
As indicated above, the blood volume in children may reach near 50% before significant changes in the blood pressure occur.
Although you are not likely to have access to urine output measurements in the field — making it more of an in-hospital monitoring situation — it is something you should be measuring if you are transporting a pediatric patient inter-facility.
Monitor with EKGs, temperature and fluids
An EKG allows you to watch for any signs of arrhythmias and pay close attention to changes in heart rate. You must be familiar with the appropriate heart rate ranges for the different pediatric age groups.
Bradycardia is an ominous sign indicating hypoxia in the pediatric patient. The pediatric patient’s cardiac output is near its maximum when the child is at rest. Therefore, children have very little room for increases.
With any increase in oxygen demands, the child will decompensate rapidly. They have very limited oxygen reserves, decreased functional capacity.
Observation of cyanosis in the pediatric trauma patient is a late sign of deterioration. Children can have a fair amount of deoxygenated blood circulating without showing signs of cyanosis.
Keeping the pediatric patient warm also is crucial because hypothermia interferes with resuscitative efforts. Pediatrics lose heat rapidly to dissipation, as they have a larger surface area to volume ratio than adults do.
It is important to provide adequate fluid resuscitation while not overloading them. Maintenance fluids — 4, 2, 1 method. Boluses should be given at a rate of 20ml/kg.
These are just a few of the things you must remind yourself of when assessing the pediatric trauma patient, while keeping in mind patients may not be able to vocalize their complaints depending on their age.
Although these calls may test you emotionally and clinically, if you maintain a strong knowledge of early recognition and treatment of the pediatric trauma patient, you can significantly decrease mortality and morbidity in this population.
Learn more about pediatric arrest in these courses
- Live Individual ALS L-5 — Cardiac Arrest Management, Pediatric Arrest Management (2 Hr)
- Live Individual ALS L-8 — Includes CHF, Pediatric Arrest, ACS (2 Hr)
Learn more about caring for pediatric injuries in these courses
- Live Individual ALS L-19 — Includes Life Span Developement, Pediatric A/P, Pediatric Seizures, Pediatric Preventable Injuries (2 Hr)
- Live Individual BLS L-3 — Includes Pediatric Transport & Airway (2 Hr)