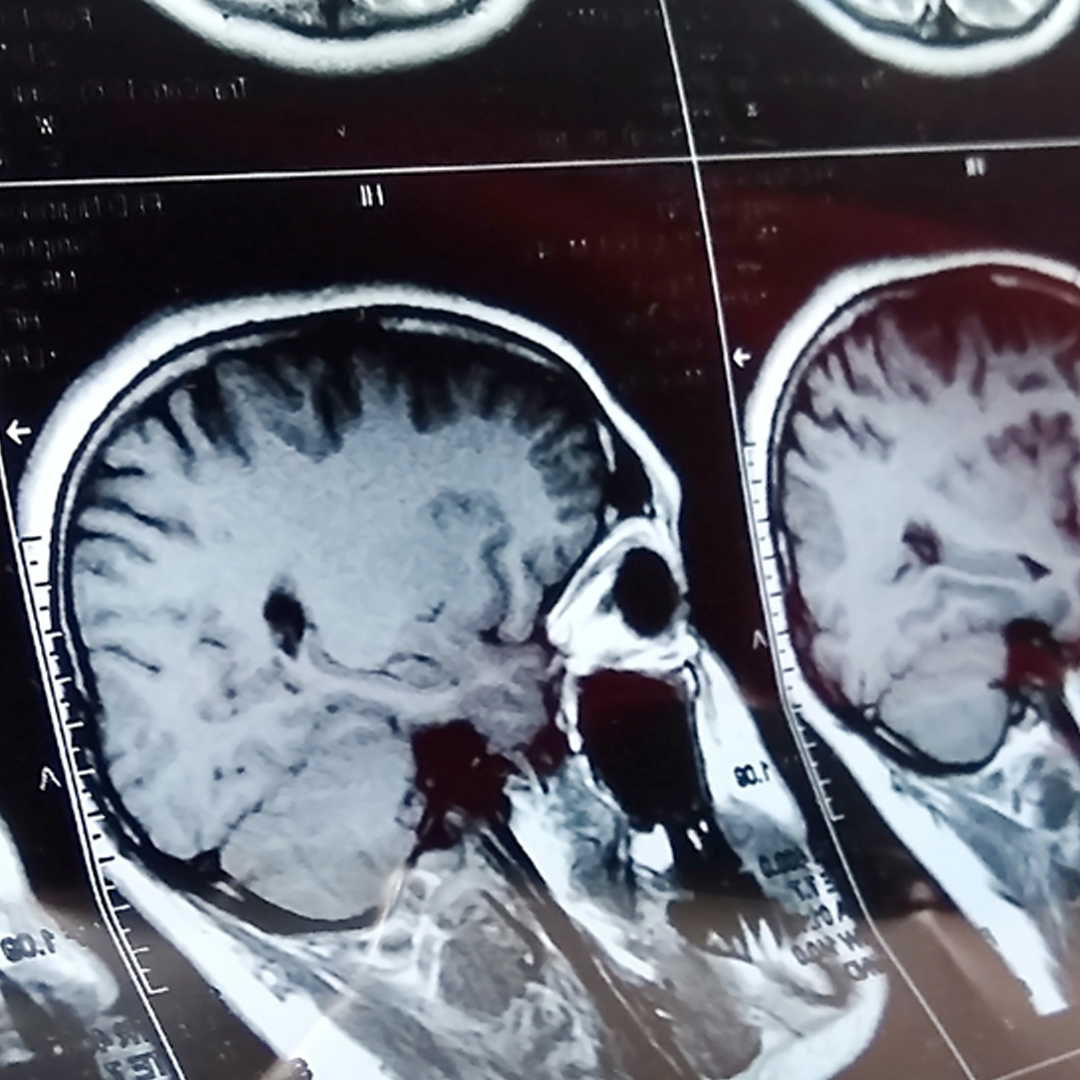
The human brain is an incredible organ. It contains billions of neurons and is responsible not only for the higher functions that set us apart from all other living things, but also is responsible for maintaining all of our life sustaining functions. It weighs about 3 pounds (approximately 2% of total body weight) yet it consumes 1/5 of our total calories and oxygen. When the brain experiences any issues with supply of these nutrients, altered mental status often ensues. The cranial vault itself is occupied by 3 parts including the brain tissue (80%), cerebral spinal fluid (10%), and blood (10%). Because the cranial vault cannot expand nor contract, the contents held inside must strike a balance between them. This is the underlying principle of the Monro-Kellie Doctrine. If one part of the cranial vault contents increases in volume, one or both of the other 2 need to decrease in volume to compensate. This relationship between the brain tissue, the CSF and the circulating blood in the cranium is what dictates intracranial pressure. The body’s ability to regulate ICP is what keeps everything we do on an even keel.
The human body produces about 500-700 ml of of CSF per day with approximately 75-100 ml of this CSF being contained in the cranium at any given time. The body will produce this same amount of CSF regardless of what the intracranial pressure level is. The body pumps about 100 liters per day into the cranial vault to perfuse the brain and at any given time, there is around 750 ml of blood in the cranium. This balance of blood, CSF and brain tissue is what produces a normal intracranial pressure range of 0-15 mm/Hg. Cerebral Perfusion Pressure (CPP) is what determines how much blood flow is delivered to the brain itself. The typical CPP is 70-90 mm/Hg. The formula for CPP is MAP (mean arterial pressure) – ICP (intracranial pressure). When the ICP increases but the MAP stays the same, CPP decreases accordingly.
So let’s put this into perspective. Think of this range as a traffic light at an intersection: CPP <50 mm/Hg is a Red Light You need to stop and address the problem immediately CPP 50-60 mm/Hg is a Yellow Light Proceed with caution because something bad may happen CPP >60 mm/Hg is a Green Light Everything is going well and you can proceed.
Not all ICP elevations are due to head trauma. Examples of medical conditions that can cause the ICP to rise are space occupying lesions like brain tumors, brain tissue swelling due to ischemia or electrolyte imbalances. If the CSF that is constantly entering the cranial vault cannot drain adequately, this can also cause an increase in ICP. Infectious processes like encephalitis or meningitis can also elevate the ICP.
Management of ICP elevation involves not only identifying and attempting to reverse the root cause but also providing interventions to assist with decreasing the ICP in an attempt to increase the CPP and minimize long term neurological damage. Something as simple as proper positioning of the patient with the head at 30-45 degrees with the head facing forward can aid in CSF and blood flow drainage from the cranial vault. Pharmacologic interventions such as Hypertonic Saline (3%-23.4%), Osmotic Diuretics like Mannitol, and ensuring adequate oxygenation via supplemental oxygen administration and ensuring adequate systemic perfusion can also aid in limiting long term damage to the brain. Avoiding temperature deviations, particularly avoiding core body temperature elevations can also be beneficial. One often overlooked stressor to neurologically injured patients is transport related stimulation. Things like ambient air temperature variations, g-forces, noise, vibration, light stimuli and rough handling can worsen neurologic outcomes.
While the brain accounts for only a small portion of our total body weight, it consumes a large amount of our body’s circulating blood flow, oxygen and glucose. Studies have shown that even a momentary drop in perfusion and/or oxygenation can increase neurological damage by 40%. What healthcare providers do (or don’t do) during the brief period we are treating the neurologically injured patient can make a huge difference in how well these patients recover. Our interventions and actions matter.